
This Impact series highlights how we support our partners to build better health systems. Here, we look at how the 45 and Up Study is being used to support integrated care.
Sir John Oldham, chair of the UK Independent Commission on Whole-Person Care, describes integrated patient care as “one person, supported by people acting as one team, from organisations behaving as one system”.
The potential benefits of streamlining healthcare in this way have caught the attention of governments around the world and in NSW, integrated care is one of three strategic directions in the State’s Health Plan: Towards 2021. In 2014 the government committed $120 million over four years to implement innovative local integrated care models across the State.
And as one of three demonstrator sites involved in the NSW Integrated Care Strategy, Central Coast Local Health District has chosen to focus its energies on streamlined care for patients with high needs, such as vulnerable aged people and those with chronic or complex conditions.
Identifying the right patients
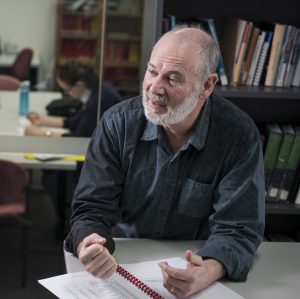
“We are trying to identify people in the community who may have underlying complex health and social issues. Then we can develop ways to help them and integrate the network of services before their health deteriorates,” says Dr Peter Lewis, Director of the Central Coast Public Health Unit.
“This is a 10-year vision. To start, it means we need to find ways to predict people in the community who are more likely to be admitted to hospital in the next 12 months. The way the health system is funded by both state and federal governments in Australia means we don’t always have a ready ability to link different sets of data compared with some other countries but the Sax Institute’s 45 and Up Study can link the hospital and Medicare parts of the picture.”
Key factors
Dr Lewis says the Study has already been used to identify some key factors that might indicate increased risk of hospitalisation, such as number of chronic conditions and number of GP visits in the previous 12 months. He and his team are working with the Institute’s Analysis for Policy program, which helps agencies use the 45 and Up Study data to answer their policy and program questions. Because the 260,000 participants in the study have answered questions such as whether they live alone and what type of support networks they have, the data can provide a much fuller picture of people’s health and social care journeys when it is linked with other information such as hospital and general practice use.
“The Study is a wonderful resource we can use to start looking at these important issues,” Dr Lewis says.
“Over the next year we plan to use the Study to inform how we select and find patients in the community before they are admitted to hospital. There are 14,000 people from the Central Coast participating in the Study but the analyses we are doing in the first instance are on the entire Study population because we need all of that information to get the best possible results. In time though, after we introduce strategies to integrate care, we will be able to measure service use in our own area.”
Find out more
- Read more about our impact in the latest Annual Report
- Learn about the 45 and Up Study
- Contact our Analysis for Policy team to see how the 45 and Up Study can help you with your policy questions





